www.theoxfordscientist.com
- First Duty
- ... the dry cough, a lethal hate crime
- ... open letter to Premier Danielle Smith
- Trump Guilty on all 34 Felony Counts
- shooting of PM of Slovakia
- YouTube channel, launch
- Carlson, tuckered out
- ... Chinese New Year - 2024
- ... orange jesus sprouts sixth finger
- ... Wagner Group in Africa
- ... conduct unbecoming an MP
- Alberta, burning
- ... the Trump legacy
- Eric LaMont Gregory
- Wacko in Waco
- Pence, Christian last
- ... Putin indicted
- The Egyptian Secret
- Fox fiction
- The Open Skies Treaty
- derailed in Ohio
- close your Twitter account
- ... espionage-a-lago
- Highland Park
- Canada bans handguns and assault rifles
- ... apology, only a first step
- ... world wide auto surf
- Conklin to Buffalo
- Danielle Smith and Liz Truss
- An End to War
- Globe & Mail, blatant sophistry
- conservative press, a fitting epitaph
- Uvalde, explanation time
- ... Ukraine, a crime against humanity
- Open Letter to Justin Trudeau
- Queen Elizabeth II
- Moscow Mitch
- ... illiberal roadshow descends on Edmonton
- ... don't cry for Kenney, Alberta
- ... Edmonton, on the world stage
- ... advertise in Chinese & English
- ... missing in Edmonton
- Human Rights
- Facebook, bankrupt ethically & financially
- Pelosi rejects Jordan
- ... vaccine roulette
- ... a mask in time saves nine
- 9/11 + 17
- the Gregory military doctrine
- lying Rodgers, unsportsmanlike Brady, falter
- ... best free traffic list 2021
- 34% of Covid survivors - will not fully recover -
- Trump ... doing Putin's bidding
- Coronavirus, a perfect storm
- Biden/Harris, ... America, can breathe, again
- ... in the heat of the day
- 11 September 2021
- Donald J Trump - like father, like son
- Jim Jordan will resign, inevitably
- ... raise money for your group
- Paris - Sanguinary excess, again
- Mitch McConnell is no Alexander Hamilton
- What Trump knew 28 January 2020
- None Dare Call It Murder
- use of force, part 2
- Coronavirus, the second wave
- Click & Join 2021
- Coronavirus Pandemic, Part 2
- Coronavirus Pandemic
- Terror Returns to London Bridge
- use of force, part 1
- Ohio's trio of shame
- ... how to earn Bitcoin
- Kenney: Scheer nonsense, part 2
- the dark charisma of Donald Trump
- the three stooges
- Trump's base, 24% and dwindling
- Scheer Nonsense
- getting away with murder
- World Wide Auto Surf
- Beyond a reasonable doubt
- Mueller, Redactions & Twitter
- An All Alberta Solution
- Obama Attends Raptors Game
- Call for action on cannabis convictions
- John Bolton: beware the Trojan horse
- Mandel Clarifies MMR Stance
- People First - Dai for Whitemud mp4
- Notley, Mandel or Kenney
- Dai for Whitemud. Dai for Alberta
- To refine or not to refine
- Trump under subpoena
- Mandel vs Elections Alberta
- Individual 1 - Donald J Trump
- Is Mississippi Learning?
- Stand Back & Stand By
- Flynn Seeks Delay in Sentencing
- Roadmap to Trump's Impeachment
- Michael Cohen sentenced
- Trump Obstructing Justice
- Defense Secretary Resigns
- The Ultimate Vanishing Act
- Hate Crimes are Increasing
- Trump announces Military Doctrine
- The Meeting, Trump Tower, June 9 2016
- 13 Angry White Male Senators
- Mean SOBs, Ryan & Jordan
- Trumpgate, a review of the facts
- Treason by the Dozens
- Terror on London Bridge
- Anti-Trump Ryan as Speaker, doubtful
- Haiti - shameful Red Cross 40% admin costs
- Deadly Bastille Day in Nice
- Special Powers
- Brussels - revenge attack
- Gregory's forte
- America First
- Brexit triumphs in UK referendum
- Ali
- Guns, Obama, the NRA & the Cleric
- Gorsuch & Brown v Board of Education
- The Generosity of America
- To Protect and To Serve
- Where is Alma Del Real?
- The Islamic World - a primer for policy makers
- The Lists - The Missing and Unsolved Homicides
- Michiana Murders
- Clinton
- Kings, Emperors & John Boehner
- Donnelly - the constant campaigner
- Kevin McCarthy
- Alberta Party
- Selections from The Ultimate Vanishing Act
- Malaysian Airlines Flight 370
- Ukraine - the Putin Doctrine
- Twilight
- Principles
- Bridge-gate: a closer look at Christie's staff
- Mandela
- Liangjun Wang
- Rethinking Syria
- about Chechnya
- Rethinking the War on Terror
- Tepid waters
- Linkage Blindness
- None Dare Call it Treason
- Emancipation
- Power
- Newtown - a cry for help
- Quarantine
- 11 September
- Hidden Crimes, Hidden Victims
- Cry, My Beloved Country
- Cruel Winds of October
- Doctrine
- Fed Video
- Under Seige
- Labor Day
- Destiny of America
- McEwen
- Rampage
- Threats
- GSK
- McEwen
- Condoleezza's watch
- Danger
- B R I C S
- Israel
- Huckabee
- Evidence
- Ties that Bind
- Sarajevo / Rwanda
- Violence
- Baby Safety
- MLK
- Libya
- Franklin
- Principles
- Fox 45
- America Wins Nobel Peace Prize
- Celina
- Middletown
- Arms Race
- Egypt
- Dollar
- 3 July
- $6 Trillion
- Jefferson and Adams
- 4th
- Libya
- Fening
- Abe
- Housing for Haiti
- Palin on Haiti
- ' ... an innocent man'
- Oil in the Gulf
- ... a wider regional conflict
- the demise of General McChrystal
- ... and to the republic
- BP and the Precautionary Principle
- Making Sense of Fort Hood
- Air Quality
- Un largo crepúsculo Lucha
- Israel
- Policy
- Home
- Casa
- un tambor diferente
- The Oxford Years
- Defense
- The Secret Hold
- INS will cease to exist
- ABC Toledo
- the grapes of wrath
- H1N1 Fluenza
- Tantamount to Treason
- MKL 4th speech
- Trans Dip
- Trump Rescinds DACA
- Rethinkin Syria
- Oxfam, IRC and other NPR Darlings
- Top Nine Articles for March 2015
- The Ultimate Vanishing Act
- Where is Alma Del Real?
- Alma Del Real
- 11 September
- A Measure of Philanthropic Success
- Tantamount to Treason
- South Carolina
- Double Crossed by Double Standards
- Call for photo radar cash grab inquiry
- Remembrance Day 2015
- Trudeau victory portends
- Blair Speech to Congress 2003
- Justin Trudeau, Tony Blair & Marijuana
- Trump, Harper, Ambrose & Ryan
- Saudi Arabia vs Iran
- The Islamic World ... the basics
- 2020 Presidential Candidate Releases Book
- Mississauga house explosion
- Reset: Driving Black in America
- Giuliani, shut up, stop name calling & prepare to govern
- Stop the Madness in Aleppo & Mosul
- Drain The Swamp
- Unpresidented
- Trump & the CIA, the high priest of false security
- The Hour of Maximum Danger
- Quebec, Queens U, Charleston & Trump
- Paul Ryan, Steve King, Trumpcare & Babies
- Harvey wreaks havoc
- VPN, don't surf without it
- Anju Sharma, the right choice for Edmonton-Mill Woods
- Adlandpro
- Trump's Iranian ties
- Brianna Keilar CNN - the big lie
- ... best free manual surf list 2021
- the Gregory military doctrine
- theOxfordscientist.com now on Tik Tok
- Chopin
- in the Course of human events
- 37 countries ban felon Trump
- un Plat qui se Mange Froid
- Trump shot at rally by 20-year-old
Governor Andrew Cuomo failed, miserably - https://www.theoxfordscientist.com/coronavirus-the-second-wave.html - click URL to read article
None Dare Call It Murder
... the availability of ECMO equipment has not kept pace with
increased ventilator treatment for pneumonia, with lethal consequences
E LaMont Gregory MSc Oxon
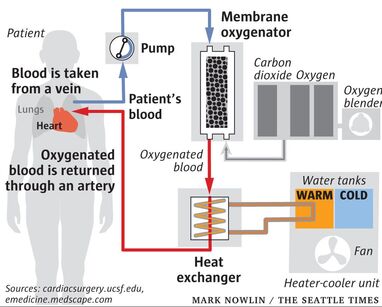
Extracorporeal membrane oxygenation (ECMO) is used as a hemodynamic support system to help maintain an
adequate supply of oxygenated blood in the body, and to allow the heart and lungs to rest in critically-ill patients.
An ECMO machine oxygenates a patient's blood outside the body, by pumping the blood through tubing
into an artificial lung, where oxygen is added and carbon dioxide is removed. The blood is then warmed
to the patient's body temperature and pumped back into the patient’s body.
Veno-Arterial, VA ECMO, is connected to both a vein and an artery when there are problems with the heart
and lungs, while Veno-Venous, VV ECMO, is connected to one or more veins, usually near the heart, and is
utilised when the problem is primarily in the lungs.
... it is a question of ethics, ultimately
Rachel Maddow of MSNBC appeared giddy as she basked in her newly acquired, albeit a sophomoric understanding of the marvel of ECMO, during her hour-long opinion piece, cum news reporting, towards the end of the week, which began on the 5th of July, 2020.
However, as discussed heretofore, Rachel Maddow, more than three months prior, had covered a news item concerning the untimely demise of a dedicated medical director of the emergency department of a prestigious Manhattan hospital, in which ECMO, or the lack thereof, can be reasonably deduced to have played a contributing role. Rachel Maddow eulogized the doctor in one segment, paraded a grieving relative in a second segment, and evolved the story into a short-lived crusade for mental health assistance for all medical workers in a third segment, before the story vanished from public view.
What we did not see from our cable-news investigative journalists and opinion framers, was one iota of an investigation into the circumstances within the hospital, and more specifically within the emergency room setting, during the raging pandemic that describes New York City hospitals leading up to the emergency room medical director's demise on the 26th of April, 2020.
However, as discussed heretofore, Rachel Maddow, more than three months prior, had covered a news item concerning the untimely demise of a dedicated medical director of the emergency department of a prestigious Manhattan hospital, in which ECMO, or the lack thereof, can be reasonably deduced to have played a contributing role. Rachel Maddow eulogized the doctor in one segment, paraded a grieving relative in a second segment, and evolved the story into a short-lived crusade for mental health assistance for all medical workers in a third segment, before the story vanished from public view.
What we did not see from our cable-news investigative journalists and opinion framers, was one iota of an investigation into the circumstances within the hospital, and more specifically within the emergency room setting, during the raging pandemic that describes New York City hospitals leading up to the emergency room medical director's demise on the 26th of April, 2020.
... normal practice, a case study
Lola S. was a thirtyish year old woman who traveled over the end of the 2019 holiday season from her home in Grand Junction, Colorado, to Arizona and then on to Las Vegas, before returning to Grand Junction just after the new year. After returning, in spite of having what she described as minor flu-like symptoms, she decided to visit her sister, who lived some 75 miles south in Montrose, Colorado.
When she arrived in Montrose Lola's flu-like symptoms worsened, progressively. So much so that her sister thought it wise to take her to the emergency room of the local hospital.
Within hours of her arrival at hospital that evening Lola was admitted, her doctors assessed probable pneumonia, and Lola was intubated and put on a ventilator.
Her condition continued to deteriorate over night, and the next morning she was transferred by air ambulance, some 260 miles northeast to a tertiary hospital in Denver. After several hours of ventilator therapy, doctors were unable to keep her blood properly oxygenated and ECMO (ELS) was initiated. This is routine practice.
ECMO, in the preponderance of cases is employed for between one-half to one hour to adequately oxygenate a patient's blood. And, in a preponderance of cases, after the heart and lungs have had a brief period of rest, ventilator therapy can be resumed, successfully.
Valiantly, doctors continued ECMO procedures in the case of Lola S., extraordinarily, but not unheard of, for almost four hours, at which time Lola S. expired.
Although unsuccessful, Lola's treatment was normal, that is, routine practice for instances when intubation and ventilation alone are unable to adequately oxygenate and remove carbon dioxide from a patient's blood, which in a healthy body is the function of one's lungs.
Lola S., is not a hypothetical case, but became the first patient in the United States, on the 8th of January 2020, to have recorded on her death certificate that pneumonia and coronavirus were contributing factors to her ultimate and premature demise.
Our interest here is to establish, by way of an example, what is normal medical practice in the treatment of pneumonia (pneumonia used here euphemistically to cover a range of conditions requiring ventilation therapy) when a patient's blood cannot be adequately oxygenated without mechanical assistance.
The 8th of January, 2020, also provides us with a date, a baseline as it were, from which we can construct an exact accounting and verifiable accounting of the ratio of pneumonia patients, ventilators and ECMO equipment available to treat them. We can also establish the ratio of pneumonia patients requiring ECMO and the success rate of its implementation.
The question then becomes, did the ratio of ECMO equipment availability keep pace with the growing number of pneumonia patients as the incidence of coronavirus related pneumonia cases increased, dramatically?
If so, medical practice, at least, from an medical equipment availability perspective in the treatment of pneumonia patients requiring mechanical assisted oxygenation, could be maintained, as per usual.
If not ...
Eulogizing our emergency medical room director, the cable news media management bureaucracy settled on the story that she was 'distraught over coronavirus'. Well, aren't we all?
Let us consider that she was a dedicated physician, who had for more than a decade not only participated in, but directed the emergency room clinical medical triage decision-making process, where patient treatment is guided solely on the best available medical evidence, as to which patients would respond to life-saving ECMO therapy.
But in no case, and under no circumstances is it ethical to simply pull the plug, so to speak.
And, consider that in the midst of a crisis of coronavirus-related pneumonia patients, you are instructed by the corporate owners of the hospital, who are somewhat disgruntled that in New York, they are being reimbursed $22,000 per coronavirus patient, while in Trump-friendly Kentucky, hospitals are being reimbursed some $357,000 per coronavirus patient, to forget about ECMO, pull the plug on patients who need it and put that ventilator on another patient.
Imagine that circumstance, if you will.
It is incumbent upon us to know the truth, and speaking with one voice ascertain that in Canada the Prime Minister, our Premiers, and Territorial leaders will not tolerate institutional murder. And, it is incumbent upon all those who practice medicine, our heroes, those that have sworn to uphold medical ethical standards, including the protection of every individuals human rights, are not involved in a conspiracy of silence.
In the United States today, there is little room for any further doubt that routine medical practice has given way to something that is unrecognizable e.g., mass graves, bodies found in the cargo area of rented trucks and intolerable disparities in the provision of medical services to racialized communities.
When she arrived in Montrose Lola's flu-like symptoms worsened, progressively. So much so that her sister thought it wise to take her to the emergency room of the local hospital.
Within hours of her arrival at hospital that evening Lola was admitted, her doctors assessed probable pneumonia, and Lola was intubated and put on a ventilator.
Her condition continued to deteriorate over night, and the next morning she was transferred by air ambulance, some 260 miles northeast to a tertiary hospital in Denver. After several hours of ventilator therapy, doctors were unable to keep her blood properly oxygenated and ECMO (ELS) was initiated. This is routine practice.
ECMO, in the preponderance of cases is employed for between one-half to one hour to adequately oxygenate a patient's blood. And, in a preponderance of cases, after the heart and lungs have had a brief period of rest, ventilator therapy can be resumed, successfully.
Valiantly, doctors continued ECMO procedures in the case of Lola S., extraordinarily, but not unheard of, for almost four hours, at which time Lola S. expired.
Although unsuccessful, Lola's treatment was normal, that is, routine practice for instances when intubation and ventilation alone are unable to adequately oxygenate and remove carbon dioxide from a patient's blood, which in a healthy body is the function of one's lungs.
Lola S., is not a hypothetical case, but became the first patient in the United States, on the 8th of January 2020, to have recorded on her death certificate that pneumonia and coronavirus were contributing factors to her ultimate and premature demise.
Our interest here is to establish, by way of an example, what is normal medical practice in the treatment of pneumonia (pneumonia used here euphemistically to cover a range of conditions requiring ventilation therapy) when a patient's blood cannot be adequately oxygenated without mechanical assistance.
The 8th of January, 2020, also provides us with a date, a baseline as it were, from which we can construct an exact accounting and verifiable accounting of the ratio of pneumonia patients, ventilators and ECMO equipment available to treat them. We can also establish the ratio of pneumonia patients requiring ECMO and the success rate of its implementation.
The question then becomes, did the ratio of ECMO equipment availability keep pace with the growing number of pneumonia patients as the incidence of coronavirus related pneumonia cases increased, dramatically?
If so, medical practice, at least, from an medical equipment availability perspective in the treatment of pneumonia patients requiring mechanical assisted oxygenation, could be maintained, as per usual.
If not ...
Eulogizing our emergency medical room director, the cable news media management bureaucracy settled on the story that she was 'distraught over coronavirus'. Well, aren't we all?
Let us consider that she was a dedicated physician, who had for more than a decade not only participated in, but directed the emergency room clinical medical triage decision-making process, where patient treatment is guided solely on the best available medical evidence, as to which patients would respond to life-saving ECMO therapy.
But in no case, and under no circumstances is it ethical to simply pull the plug, so to speak.
And, consider that in the midst of a crisis of coronavirus-related pneumonia patients, you are instructed by the corporate owners of the hospital, who are somewhat disgruntled that in New York, they are being reimbursed $22,000 per coronavirus patient, while in Trump-friendly Kentucky, hospitals are being reimbursed some $357,000 per coronavirus patient, to forget about ECMO, pull the plug on patients who need it and put that ventilator on another patient.
Imagine that circumstance, if you will.
It is incumbent upon us to know the truth, and speaking with one voice ascertain that in Canada the Prime Minister, our Premiers, and Territorial leaders will not tolerate institutional murder. And, it is incumbent upon all those who practice medicine, our heroes, those that have sworn to uphold medical ethical standards, including the protection of every individuals human rights, are not involved in a conspiracy of silence.
In the United States today, there is little room for any further doubt that routine medical practice has given way to something that is unrecognizable e.g., mass graves, bodies found in the cargo area of rented trucks and intolerable disparities in the provision of medical services to racialized communities.
... Ragusa 1377
On the 27th of July, 1377, the City Council of the eastern Adriatic port municipality of Ragusa (modern-day Dubrovnik) enacted an ordinance stipulating 'that those who come from plague-infested areas shall not enter Ragusa, or its district, unless they spend a month on the islet of Mrkan or in the town of Cavtat, for the purpose of disinfection.'
Mrkan was an uninhabited rocky island south of the city and Cavtat was situated at the end of the caravan road used by overland traders en route to Ragusa.
And thus, the port city Ragusa became the first to pass legislation requiring the mandatory quarantine of all incoming ships and trade caravans in order to screen for infection.
... Lyon 2020
in process - bookmark this page - ctrl + D